Menière’s Disease
“Cochlear” Menière’s and “Vestibular” Menière’s
Causes
Diagnosis of Menière’s Disease
Symptoms
Testing
Disease Progression
Drug and Diet Treatment
Surgical Treatment
Conclusion
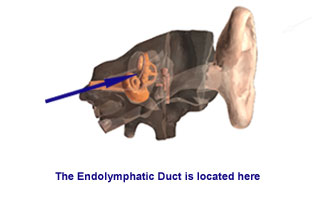
In order to better understand Menière’s Disease, it is important to have a general knowledge of the structure and function of the inner ear . Normally, the fluids of the inner ear circulate. They are produced, circulated and are cleared by absorption. In Menière’s Disease, either an overproduction, or an under absorption, of endolymph (fluid) produces a “plumbing problem”: the over accumulation of endolymph backs up under pressure, resulting in a bulging of the endolymphatic chambers.
“Cochlear” Menière’s and “Vestibular” Menière’s
It was once thought that Menière’s Disease could be categorized as either “Cochlear” (just hearing loss) Menière’s or “Vestibular” (just vertigo) Menière’s. It is now believed that there is only one Menière’s Disease, and that those patients with either cochlear or vestibular symptoms eventually develop the full syndrome.
Causes
Menière’s Disease is a condition that has no known cause. Menière’s Syndrome refers to the same disease, but for which a recognized cause is suspected. Potential causes of Menière’s Syndrome include allergy, endocrine-metabolic disorders, syphilis, immune mediated disorders, congenital malformations, etc. The fact that Menière’s Syndrome can be traced to specific causes makes treatment easier.
Diagnosis of Menière’s Disease
Diagnosis begins with a general physical examination and otologic (relating to the ear) evaluations. In late stages of the disease, some abnormalities of equilibrium can be detected by neurologic (relating to the nervous system) examination.
Special tests are necessary to diagnose Menière’s Disease. The symptoms of Menière’s Disease are neurologic (related to the brain). A long list of possibilities must be ruled out before the diagnosis of Menière’s Disease can be made. A number of tests used to diagnose Menière’s Disease reveal what the condition is not, helping health care providers go through a process of elimination.
Symptoms
Most Menière’s Disease patients experience all of the classic symptoms: Patients experience periods of fullness or ear pressure followed by loud, roaring tinnitus (head noise) and hearing loss. These events occur from minutes to days or weeks before an acute attack of vertigo. It is these symptoms that constitute an “aura” or warning that a disabling attack of vertigo is about to occur. Vertigo is a spinning, whirling sensation, even while standing still. Profuse sweating, nausea, vomiting and even loss of bowel or bladder control can result from such a vertigo attack. Vertigo typically lasts ten minutes to an hour; the entire attack often encompasses hours. Hearing returns to normal after an attack and the pressure and tinnitus go away. There is an initial period of drowsiness.
Menière’s patients are sensitive to changes in weather. The diseased, fluid-filled inner ear is very sensitive to barometric pressure changes. For this reason, spring and fall are “bad seasons” for sufferers. Hormonal changes, such as those caused by menstrual cycles and pregnancy, may aggravate Menière’s sufferers. Among other things, nicotine is a drug that affects the inner ear microcirculation.Cigarette abuse worsens Menière’s Disease. Tension, stress, anxiety, and exhaustion are known to provoke attacks or limit disease control by treatment.
Testing
In Menière’s patients, testing of the hearing sense reveals low frequency, sensori-neural hearing loss. Speech understanding is generally normal (80-100%). The hearing impairment caused by Menière’s Disease may increase sensitivity to sound, making ordinary sounds painful or uncomfortable. It also may cause a disturbed perception of pitch, so that one tone sounds like two tones.
Electrocochleography (ECoG) is a special test, claimed by some to be of use in diagnosis and monitoring Menière’s Disease. The patient wears earphones, which provide a “click” stimulus to the inner ear. Sophisticated computer technology enables examination of the inner ear’s response to this stimulus. The response has been shown to be characteristically abnormal in Menière’s Disease.
Auditory brainstem response (ABR) audiometry is an established test, commonly suggested to Menière’s patients. Like ECoG, earphones present a click stimulus to the ear. Electrodes taped to the scalp, and averaged by computers, record the response to these stimuli.
Vestibular Testing Dizziness is not a symptom that a health care provider can examine physically. Vestibular tests help assess dizziness.
The semicircular ear canals can be stimulated using heat. Exposing the ear to warm and cool water produces a flow movement of endolymph in the balance canals that stimulates the hair cells and the balance nerve. Impulses travel to the brainstem, triggering reflexes that produce an alternating slow and quick eyeball motion. The eyeball motion can be recorded electrically as an ENG (electronystagmography), which is similar to an EKG or EEG. In Menière’s Disease, normal or slightly reduced responses are noted on ENG. As the disease progresses, more serious ENG abnormalities can occur.
Special Testing
- If allergy is suspected, allergy testing may be required.
- Testing for syphilis may be required, since later stages of syphilis can affect the central nervous system, including the inner ear
- Testing for immune mediated disease of the ear may be required, and has nothing to do with AIDS. In this condition, the body’s defense mechanisms turn against it and attack the ear. In addition to other problems, Menière’s Syndrome may result.
- Endocrine-metabolic disorders (diabetes, thyroid and hormones) may be surveyed as a potential cause of Menière’s Syndrome.
Disease Progression
The behavior of Menière’s Disease is totally unpredictable. Following an attack, the Menière’s sufferer may not have one again for 15 years or more. This is characteristic. On the other hand, this disease may be rapidly progressive – destroying hearing and balance in weeks to months.
As the disease progresses, episodes usually become more frequent. As a result, the tendency for hearing to return to normal after an attack becomes less and less. Hearing loss continues to occur. Tinnitus (head noise) and fullness become near constant. This course can stretch out over years resulting in near total destruction of the hearing in the diseased ear.
Vertigo attacks (dizziness) result from the deterioration in hearing. Dizzy spells occur more frequently and can be more severe. In the late stages of the disease, the condition of vertigo may vary. The patient may be constantly unsteady, with near daily vertigo attacks, or his disease may “burn out.” The latter is used to refer to the condition when the ear is virtually destroyed by the disease. While there is no vertigo or unsteadiness, total hearing loss occurs.
Personality disorders are quite common in Menière’s patients. Menière’s patients tend to be tense, and attacks are often caused by stress. As the disease progresses, patients may become withdrawn, obsessive and neurotic. It was once thought that this behavior was the result of psychiatric disorder. It is now accepted that the consequences of Menière’s Disease, both social and personal, cause negative patterns of behavior often characterized as the “Menière’s Personality.”
Very much like the loss of a loved one, the symptom complex of Menière’s Disease is something to which the patient must react. The normal patterns of anger, denial, rationalization and acceptance are typical. Individual reactions will vary, with some being quite normal, and some quite drastic. Professional or peer support is often useful as the Menière’s sufferer adjusts his life to cope with the impact of his disease. Awareness of these problems often helps in avoiding them.
Drug and Diet Treatment
Many treatment options are available for Menière’s sufferers, and some are controversial. In general, there are non-surgical treatment methods and surgical methods. Non-surgical treatment is aimed at reducing the fluid overpressure in the endolymphatic system. This is best accomplished by reducing the overall total body fluid volume. Salt restriction and diuretics (increasing urination) are prescribed. About 80% of patients are made comfortable without surgery, while about 20% are candidates for surgical treatments. In general, surgery for Menière’s Disease is reserved for those patients who have failed other treatments. In most cases, it is the vertigo that is addressed by surgical methods.
Diet
Salt restriction is useful because sodium (salt) causes the body to retain fluid. This means avoiding potato chips, pretzels, peanuts, sausage, bacon, ham, corn chips, soy sauce, salted crackers and other salty foods. Cooking with minimal salt is usually permitted, though a salt substitute is recommended for use at the table. Once stabilized, Menière’s patients become so intolerant of salt that attacks can be caused by just a small amount of salt intake.
Diuretics
Diuretics (medications that cause urination) can produce dramatic effects on Menière’s symptoms, particularly pressure and fullness. This can also help reduce the degree of hearing changes experienced. Often, salt restriction and diuretics are enough to control all Menière’s symptoms.
Labyrinthine Sedatives
It sometimes is necessary to treat Menière’s patients with labyrinthine sedatives to control vertigo. Several common medications for vertigo, such as Bonine™, Dramamine™, Bucladin™ and Antivert™ are often not very effective in Menière’s Disease. Diazepam (Valium™), however, is reported to have significant action at the inner ear level as well as in central balance pathways. It is regarded as an effective dizziness suppressant. Drowsiness is a potential side effect requiring a change in the dosage. Alertness precautions should be followed. Addiction limits long-term use.
Anticholinergic Drugs
Anticholinergic drugs are also thought to be useful. Probanthine™ and Robinul™ are popular medications. Scopolamine patches for this prolonged use purpose is discouraged. Injection of these drugs in an office or hospital setting is useful for acute attack control.
Gentamycin
Gentamycin is an antibiotic that is toxic to the balance portion of the inner ear. It can be given through the eardrum in the office by making a small hole in the eardrum. Repeated treatments are often required and it is generally less successful than surgery to stop the vertigo.
Surgical Treatment
Hearing level is considered when deciding upon a surgical procedure. When the patient is capable of hearing without or with amplification, a surgical approach that spares hearing is usually recommended. Otherwise, a “destructive” procedure may be suggested. The status of the opposite ear is an important consideration as well. If the ear opposite the hearing ear is totally dead (a dead ear), the hearing ear is usually preserved.
Bilateral disease makes the situation very complicated, so no generalizations can be made about treatment. One trend is to avoid all destruction procedures as a result of the success of cochlear implantation. Nonetheless, most agree that these procedures still have a definite place in the case of Menière’s Disease. All surgery for Menière’s Disease is microsurgical (on a microscopic level).
Labyrinthectomy
Drilling away the balance portion of the inner ear is a destructive procedure. Hearing is lost because of the interruption of ear fluid motion. The procedure is reserved for those patients in the last stages of their unilateral (affecting only one side) disease when hearing has been essentially destroyed.
Successful results are achieved in 95% of the patients undergoing labyrinthectomy. Menière’s vertigo is gone, but unsteadiness may persist until the Central Nervous System (CNS) can make up for the loss of a balance organ. In patients under age 40, compensation occurs quickly. Patients who are 40-60 years of age compensate less quickly, while patients older than 60 do even more poorly. Regardless of age, most patients move with security by 6 months after their operation. The hospital stay is generally 3-5 days. Missed work time varies for age, but for the young, it is usually less then 3 weeks. A patient over 60 may have momentary imbalance after moving abruptly for the rest of his or her life.
Endolymphatic System Surgery
This is a conservation operation in which hearing is preserved. It is commonly referred to as the “shunt” procedure. It is the only operation for Menière’s Disease that addresses the problem of hearing loss as well as vertigo.
Endolymphatic system surgery is regarded as minor, with hospital stays rarely longer than 2 nights. The procedure is low risk and offers relatively limited success, so many centers view it as a first step before getting into more involved vestibular procedures.
Vestibular Nerve Section
The balance portion of the eighth cranial nerve can be sectioned, while preserving the hearing portion. This is known as a vestibular nerve section (VNS). VNS is a more complicated operation than endolymphatic system surgery, but reported results are reliable and approach those for labyrinthectomy, while preserving hearing. VNS is an intracranial (within the skull) procedure, performed by various routes.
Regardless of the route used, in all VNS procedures, the vestibular nerve is divided to interrupt the abnormal signals being sent to the brain by the Menière’s diseased inner ear. Although hearing is monitored throughout, the operation will bring on hearing loss in 5% of patients. Other complications include those related to Cerebral Spinal Fluid (CSF) leakage and a major neurosurgical craniotomy. Hospital stays average 5-7 days. The recovery period is similar to that for labyrinthectomy
There have been countless other types of surgical options proposed over the years. These include ultrasonic irradiation and cryogenic freezing of the labyrinth. While some surgeons still perform these operations, they are not as commonly performed as the ones discussed. Research is constantly undertaken and new operations proposed for the control of this very poorly understood disease. Until the cause of the problem is discovered, it is unlikely that there will be a cure. Therefore, in most cases diuretic and salt restriction therapy is continued, even after surgery.
Conclusion
Menière’s Disease patients must seek physicians who understand their disease and who can deal successfully with it. Even without a cure, patients must know that there are options to improve their lifestyle. Peer support through networks such as the EAR Foundation’s Menière’s Network and menieres.org are an important adjunct to professional treatment. Coping strategies can be shared. Patients should understand that they are not in this alone.
Menière’s Disease sufferers can be helped. They can lead normal and productive lives. The realization of this goal depends upon a physician who understands the disease and how to manage it, and the patient’s willingness and ability to assume responsibility for his or her own well being.
For more information:
Go to the Ear, Nose, and Throat Disorders health topic.